Overview
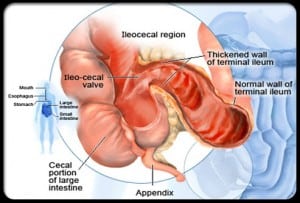
Crohn’s disease is a chronic inflammatory condition that affects the gastrointestinal tract. Classified as an inflammatory bowel disease (IBD), it can cause inflammation anywhere from the mouth to the anus, with the most common sites being the end of the small intestine (ileum) and the beginning of the large intestine (colon). Individuals with Crohn’s disease experience a range of symptoms, including abdominal pain, blood in stool, mouth sores, diarrhea, rectal bleeding, weight loss, fatigue, and fever. There can also be periods of remission. Crohn’s disease can hereditary but most people don’t have a family history. Risk factors can include age, ethnicity, family history and history of smoking cigarettes. There are a few types of Crohn’s affecting different parts of the digestive tract.
- Ileocolitis, the most common form of Chrohn’s, which affects the small and large intestine.
- Ileitis, which only affects the ileum.
- Gastroduodenal Crohn’s disease, which affects the stomach and duodenum.
- Jejunoileitis, which affects the upper half of the small intestine called the jejunum.
- Crohn’s Colitis, which affects only the colon (large intestine).
How is it diagnosed?
Endoscopic procedures such as colonoscopy, capsule endoscopy and upper endoscopy allow visualization of the gastrointestinal tract to identify inflammation, ulcers and other abnormalities. Biopsies can be taken to confirm Crohn’s. Imaging scans such as CT scans or MRIs may also be used to evaluate the extent and severity of inflammation and detect complications like fistulas. Blood and stool tests help assess markers of inflammation, anemia, and nutritional deficiencies.
How is it treated?
Crohn’s can significantly impact quality of life and requires ongoing management. While there is no cure, treatment for Crohn’s disease aims to reduce inflammation, control symptoms, and improve quality of life. This often involves a combination of medications, lifestyle modifications, and, in some cases, surgery. Medications may include anti-inflammatory drugs, immunosuppressants, biologic therapies, antibiotics, and symptom-relief medications. Lifestyle changes such as avoiding trigger foods, stress management, quitting smoking, regular exercise, and adequate hydration can help manage symptoms and improve overall well-being. In severe cases or when medications fail to provide relief, surgery can be an option to remove damaged portions of the intestine or alleviate complications such as strictures, fistulas, or abscesses. Your physician will discuss which treatment works best for you.
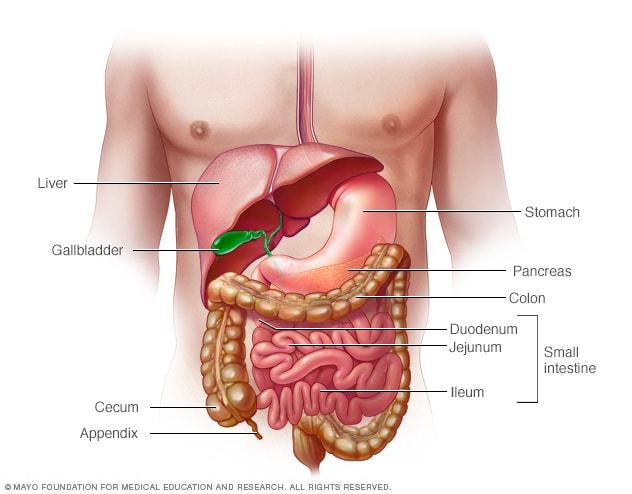
Image courtesy of Mayo Clinic
Helpful Link
https://www.crohnscolitisfoundation.org
The Crohn’s and Colitis Foundation website is a great resource on treatment options, IBD medications guide, information on diet and nutrition, research information, financial and insurance material and community support options.
References
Crohn’s & Colitis Foundation. (n.d.) What is Crohn’s Disease? https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-crohns-disease/diagnosis-testing
Mayo Clinic. (2022). Crohn’s Disease. https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304


