An EGD, also known as an upper GI tract endoscopy, is a procedure that uses a lighted, flexible endoscope to see inside the upper GI tract. The upper GI tract includes the esophagus, stomach, and duodenum—the first part of the small intestine. This procedure can be used to remove stuck objects, including food, and to treat conditions such as bleeding ulcers. It can also be used to biopsy tissue in the upper GI tract to check for conditions such as Celiac disease, and determine the causes of abdominal pain, nausea, vomiting, anemia, acid reflux or swallowing difficulties. Before the procedure, you will need to follow prep instructions given to your physician which you need to follow carefully. During the procedure, you will receive IV sedation then the endoscope with a small camera inserted down the esophagus and into the stomach and duodenum. Images are viewed on a screen, allowing examination of the intestinal lining. Biopsies may be taken, which are sent to the lab for testing. As with any procedure, the risks are small but can include perforation in the stomach, duodenum or esophagus and bleeding from the biopsy site. After your procedure, you generally can resume a normal diet but you are not allowed to drive after the procedure due to anesthesia. You will need someone to drive you to and from the center. You will be notified of your biopsy results in 1-2 weeks.
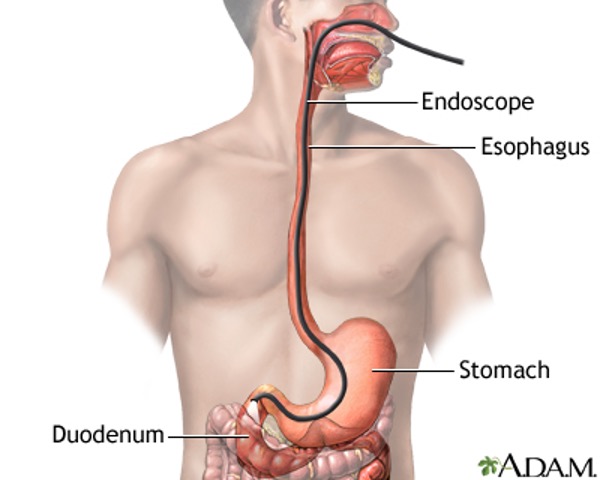
Image courtesy of Medline Plus
Reference:
Medline Plus-National Library of Medicine. 2023. EGD. https://medlineplus.gov/ency/article/003888.htm


